Clozapine: a cautionary tale
16 Oct 2024
Case study
Mr A recently started attending Dr F’s practice for a variety of minor conditions. Mr A requested a script for clozapine on his most recent visit, mentioning he had left the care of his psychiatrist months ago. Having satisfied himself that the patient had been taking the same dose long-term to treat his schizophrenia, Dr F issued Mr A his Pharmaceutical Benefits Scheme (PBS) streamlined authority prescription. The local community pharmacy dispensed the medication. A month later, Dr F and the pharmacy received correspondence from Mr A’s previous psychiatrist warning them of the special requirements for prescribing, monitoring and dispensing clozapine, which they were unaware of. When Mr A later presented with a sore throat and fever, Dr F requested a blood count, and both Dr F and the pharmacist were relieved they were able to withhold treatment in time to prevent severe medication-induced agranulocytosis.
Discussion
Clozapine is indicated for use in treatment-resistant schizophrenia, where a patient has not responded adequately to two other antipsychotics. It is effective for the treatment of the positive symptoms of schizophrenia, but requires careful initiation and monitoring due to the risk of a constellation of serious side effects such as agranulocytosis and myocarditis. It is a psychiatrist-initiated medication, but has become available to patients through their general practitioners and community pharmacies, following the introduction of shared care prescribing arrangements across states and territories within Australia. Practitioners and pharmacists must be aware of their obligations when prescribing and dispensing clozapine.
Initiation
Clozapine is typically initiated by a consultant psychiatrist within a hospital setting. Patients must be registered with a separate brand-specific clozapine monitoring service within Australia (ClopineCentral®; CPMS®; Juno Connected®) before treatment can be started. There may be jurisdictional brand preferences – Clopine® is used in Western Australia and Clozaril® in South Australia. Advice should be sought if a patient moves jurisdictions and the supply of their existing brand of clozapine cannot be continued, given the risks to monitoring continuity.
Prescribers, clinics and pharmacies must register
Prescribing medical practitioners, dispensing pharmacists, hospitals and other health facilities (GP clinics, community mental health clinics) must also be registered with the appropriate monitoring system under the central network. There may be various defined roles under the networks, including registered dedicated coordinators who oversee the programs.
Patients need regular monitoring
Registration ensures regular monitoring of the patient’s white cell count and neutrophils at specific intervals during and after the initiation period, as results must be entered into the system. The manufacturer will alert the registered centre if the patient is overdue for blood tests. Regular monitoring allows early detection of emerging neutropenia, preventing progression to potentially life-threatening agranulocytosis. Some states have developed specific clozapine initiation guidelines that require additional parameters for monitoring, such as the QT interval, CRP, and troponin levels with respect to myocarditis.
Patients who discontinue treatment for three months, or those starting treatment at a new centre, will need to be re-registered. Medical practitioners must re-register each time they relocate their practice to a different clozapine centre, or register at each clozapine centre in which they work.
PBS approvals are required
Clozapine is a section 100 highly specialised drug under the PBS. Accredited hospital-based prescribers can prescribe clozapine for both initiation and maintenance purposes. A PBS authority approval is required for most highly specialised drugs listings, and for increased quantities and repeats. Accredited general practitioners can prescribe maintenance clozapine under the PBS community access arrangements and a streamlined authority is available when prescribing at PBS-listed quantities and repeats. The PBS criteria for continuing treatment requires that authorised treating medical practitioners act under the supervision and agreement of the treating psychiatrist, who is responsible for reviewing the patient at regular intervals.
Prescribers may need authorisation
Medical practitioners should be aware of any additional state regulations that must be met before they prescribe clozapine to patients. Clozapine is a schedule 4, regulated restricted medicine under the Medicines and Poisons (Medicines) Regulation 2021 in Queensland. Only consultant psychiatrists and supervised psychiatry registrars are permitted to initiate or alter the dosage of clozapine. All other practitioners wishing to prescribe require approval from the Chief Executive Queensland Health. Further enquiries about specific requirements should be directed to the relevant medication approval and regulatory unit in the practitioner’s state.
Summary
Clozapine can be a life-changing medication for patients who have treatment-resistant schizophrenia, but it requires strict monitoring due to its side-effect profile. General practitioners and community pharmacists need to be aware of their additional obligations when prescribing and dispensing clozapine in the community. These include registering with the brand-specific clozapine patient monitoring system, obtaining PBS authority, and obtaining approval to prescribe from the relevant regulatory authority by state and territory where required.
Stay updated with the latest medico-legal content |
Subscribe to MDA National’s biannual Member publication, Defence Update, for the latest medico-legal updates, articles and case studies.

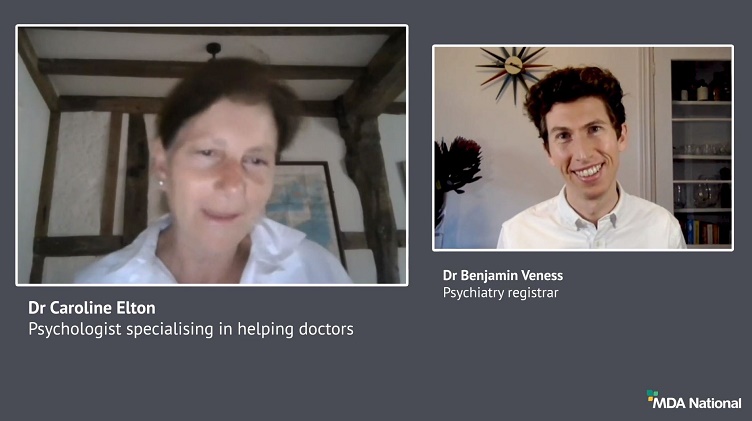
Doctors Let's Talk: Get Yourself A Fricking GP
Get yourself a fricking GP stat! is a conversation with Dr Lam, 2019 RACGP National General Practitioner of the Year, rural GP and GP Anesthetics trainee, that explores the importance of finding your own GP as a Junior Doctor.
25 Oct 2022
Systematic efforts to reduce harms due to prescribed opioids – webinar recording
Efforts are underway across the healthcare system to reduce harms caused by pharmaceutical opioids. This 43-min recording of a live webinar, delivered 11 March 2021, is an opportunity for prescribers to check, and potentially improve, their contribution to these endeavours. Hear from an expert panel about recent opioid reforms by the Therapeutic Goods Administration and changes to the Pharmaceutical Benefits Scheme.
14 May 2021
Diplomacy in a hierarchy: tips for approaching a difficult conversation
Have you found yourself wondering how to broach a tough topic of conversation? It can be challenging to effectively navigate a disagreement with a co-worker, especially if they're 'above' you; however, it's vital for positive team dynamics and safe patient care. In this recording of a live webinar you'll have the opportunity to learn from colleagues' experiences around difficult discussions and hear from a diverse panel moderated by Dr Kiely Kim (medico-legal adviser and general practitioner). Recorded live on 2 September 2020.
05 Oct 2020