Managing patient complaints
14 Dec 2024
Why do patients complain?
Patients most commonly complain because they want:
- to be ‘heard’ and express dissatisfaction at how they were treated;
- an apology and/or explanation;
- to stop it happening to someone else; or
- a refund.
Documented policy and procedures
You should have written complaint management policies and procedures – including a commitment to effectively manage complaints; process workflows and step-by-step instructions for staff; staff responsibility and delegation; timeframes; behaviour expected of staff and complainants; how to manage unreasonable conduct from complainants; the health and safety of staff; informing patients about how to make a complaint; documentation of complaints; and review of complaints to identify trends and system improvements.
Staff can be involved in creating the policy; and should have easy access to the documents and be trained in the processes. Training in customer service, managing difficult conversations, conflict resolution and cultural safety will also be helpful. Complaint handling can be stressful, and staff should be offered support.
Responding to direct complaints
The effectiveness of direct resolution may determine whether the grievance will end there, or will go further through a formal complaint process or legal action.
Verbal complaints – initial response
- Listen without interrupting and maintain eye contact (if face to face).
- Try to understand the patient’s view and respond with empathy. Treat the patient with courtesy and respect, and show that you take the complaint seriously.
- Check that you have understood by repeating back or asking questions.
- Although it’s natural to experience some initial defensiveness, try not to come across as defensive or dismissive.
- Ask the patient what they believe should have happened, and what they want to happen now. This may clarify the reason for the complaint and determine an appropriate response.
- If the complaint is complex, it may be best to ask the patient to put their concerns in writing.
- Tell the patient what will happen next and provide realistic timeframes. If the complaint relates to clinical care, it’s best that the doctor responds directly to the patient as soon as possible.
Written complaints – initial response
Acknowledge the complaint promptly, and outline next steps and timeframes. You don’t need to respond in detail immediately, but you should acknowledge that the complaint has been received and will be acted upon. Delays in dealing with complaints can add to tension and generate further resentment.
Resolving the complaint
Record all complaints, and keep notes of all meetings, phone calls and any correspondence in relation to the complaint. Store these documents separately from the patient’s medical records – although if the complaint is clinical in nature, it may be relevant to include some factual clinical information for continuity of care. A complaint should be treated confidentially and stored securely in accordance with privacy laws. If the complaint is from a patient’s relative or other source, do not respond without authority from the patient.
Triage the complaint, and decide who should review and respond.1
Be objective and fair in reviewing the complaint and considering potential remedies or actions. Give the complainant regular updates on the progress of their complaint, and an explanation for any delay.
Communicate the outcome. It might be appropriate to invite the patient to meet with you to discuss the issues – although often, if the complaint was made in writing, it is best to respond in writing.
When responding in writing, take care to address the specific issues raised in the complaint. Use plain language, avoiding jargon or medical terminology. Be open and honest, including apologising when appropriate – see the Australian Open Disclosure Framework: Saying sorry – A guide to apologising and expressing regret during open disclosure.2 Provide information about the options available to the complainant, if they are not satisfied with your response.
Reflect on the complaint, looking for what could have been done better and how lessons could be applied to the practice and its processes.
Formal complaints
If you receive a formal written complaint via a dedicated health complaints body (such as Ahpra, the Office of the Health Ombudsman or the Health Care Complaints Commission) or a broader complaints body (such as the Office of the Australian Information Commissioner), you must notify your medical indemnity insurer.
Each complaints body will have a formal process which you must comply with. There are a wide range of timeframes and possible outcomes. The complaint may be dealt with relatively quickly and be closed with no further action; or it may result in a series of assessments, audits and/or hearings which may ultimately result in disciplinary action on your medical registration.
MDA National’s Cases and Advisory Services team can help you understand the process and assist you with matters that trigger the policy. You may be invited to an interview or case discussion, but often a written response or submission is the first step.
When preparing a written response, you should:
- carefully review the complaint and medical records
- use a professional tone
- express empathy for the patient’s concerns or disappointments. Phrases such as “I am sorry you are upset…” are not an admission of liability, and do not require the expression of guilt or wrongdoing
- address any misperceptions or inaccuracies expressed in the complaint by summarising the events as you know them. Be concise, but address each of the issues raised. It may be useful to summarise the events and then use headings to address the allegations or complaints not already answered in the summary
- if appropriate, advise the patient what steps have been taken to prevent a similar event from occurring in the future, and thank the patient for bringing their concerns to your attention.
A formal complaint can be very confronting, and the process may be lengthy. You can seek support from your GP, colleagues, family and friends, MDA National, or the Doctors’ Health Advisory Service in your state or territory.
Legal and professional requirements
Good Medical Practice: a code of conduct for doctors in Australia:3
Patients who are dissatisfied have a right to complain about their care. When a complaint is made, good medical practice involves:
4.12.1 Acknowledging the patient’s right to complain
4.12.2 Providing information about the complaints system
4.12.3 Working with the patient to resolve the issue, locally where possible
4.12.4 Providing a prompt, open and constructive response, including an explanation and, if appropriate, an apology
4.12.5 Ensuring the complaint does not adversely affect the patient’s care. In some cases, it may be advisable to refer the patient to another doctor
4.12.6 Complying with relevant complaints law, policies and procedures
4.12.7 Reflecting on the complaint and learning from it.Victorian complaint handling standards under the Victorian Health Complaints Act 2016. Accredited health services under the National Safety and Quality Health Service Standards must have a complaint-handling system and processes. The right to make a complaint and provide feedback is included in the Australian Charter of Healthcare Rights. Australian Standard AS 10002:2022 Guidelines for complaint management in organisations.
- Ahpra: Checklist for practitioners handling feedback and complaints
- MDA National: The doctor or the practice – who should respond to a patient complaint
- MDA National: Managing negative reviews
- NSW Ombudsman: Managing unreasonable conduct by a complainant
Reference
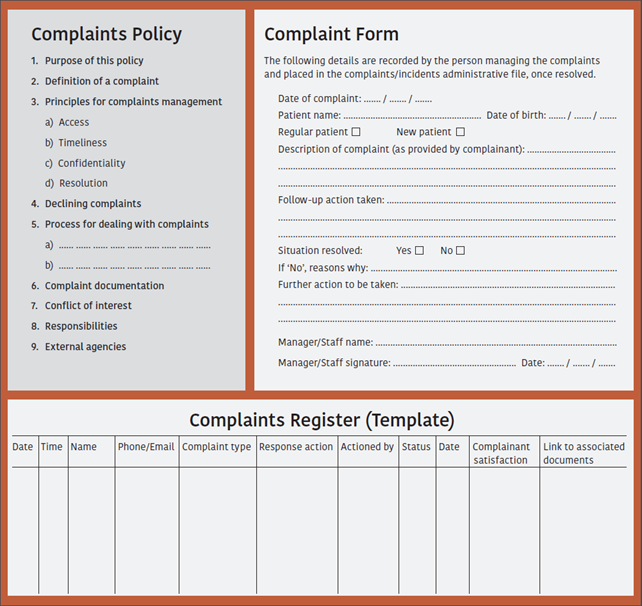
SAMPLE DOCUMENTS – Complaints Management
Stay updated with the latest medico-legal content |
Subscribe to MDA National’s biannual Member publication, Defence Update, for the latest medico-legal updates, articles and case studies.

Doctors, Let's Talk: Setting Boundaries At Work
A conversation with Nicola Campbell, Psychiatry Registrar, that explores the necessity of setting professional boundaries as a Junior Doctor.
07 Dec 2022

Doctors, Let's Talk: Your Support Network Is Your Net-Worth
A conversation with Nidhi Krishnan, Paediatric Registrar, that explores the value of building a strong network as a Junior Doctor.
07 Dec 2022

Doctors, Let's Talk: Are Retreats Worth The Money?
A conversation with Dr Emily Amos, General Practitioner, International Board Certified Lactation Consultant, and registered mindfulness teacher, that explores the utility of mindful retreats and self-care among Junior Doctors.
07 Dec 2022

Doctors, Let's Talk: Is Quitting Medicine Ever The Answer?
A conversation with Dr Ashe Coxon, General Practitioner, career counsellor, and founder of Medical Career Planning, that explores the issue of dealing with career uncertainty as a Junior Doctor.
07 Dec 2022


