Correcting or deleting medical records
23 Jul 2024
Case study
Dr Scott receives an angry email from a former patient. Dr Scott was involved in Tracey’s care when she was diagnosed with schizoaffective disorder during an inpatient stay. Her mood stabilised following treatment with an antipsychotic.
Tracey says she wrote to the practice, asking them to remove a diagnosis from her medical record because she doesn’t agree with it. The practice said no.
Tracey is asking for a complete copy of her medical record, and she again asks for her mental health diagnosis to be removed. Tracey is going through a custody dispute with her ex-husband and doesn’t want him to subpoena the notes.
When Dr Scott reviews the record, she notes a very long entry made by a receptionist following a confrontation that led to Tracey being banned from the practice.
Discussion
The practice is correct, insofar as it is not appropriate to correct or delete the diagnosis from Tracey’s medical record. But is it enough to just refuse?
Requests to correct or delete records
You must take reasonable steps to correct health information you hold about a patient, if you are satisfied the information is incorrect and the patient asks you to correct the information. Health information may be incorrect if it is inaccurate, out-of-date, incomplete, irrelevant or misleading.
The Guide to Health Privacy published by the Office of the Australian Information Commissioner (OAIC) has an excellent flow chart in Chapter 5, page 4, and your privacy policy should provide information to patients on how they can request a correction to their health information.
Requests for correction may relate to factual information that can be easily amended. If the information is incorrect, you should take steps to notify other entities of the correction, provided it is practicable to do so.
If the request is more complex, and refers to clinical information or diagnoses, it may be more appropriate to invite the patient to “associate a statement”.
According to the OAIC, “…your medical opinion is not inaccurate just because a patient disagrees with it. Your opinion may be ‘accurate’ provided you present it as an opinion, it accurately records your view, and takes into account competing information and views.”
If you consider the information does not require correction or deletion, you must provide written notice of your decision not to correct or delete health information within 30 days, detailing:
- the reason for the refusal;
- the patient’s option to associate a statement; and
- avenues for complaint if the patient is unhappy with the decision.
In the first instance, you can invite the patient to make a formal complaint to the practice. If the patient is not happy with the response from the practice, they can escalate the complaint to the OAIC or a health complaints body.
Associating a statement
If patients don’t agree with a diagnosis or a clinical finding, you can invite them to “associate a statement” which is kept on the medical record in a way ‘that makes it apparent to other users of the health information’. The OAIC recommends the statement not be more than one page in length.
Requests to delete records
It would be unusual for medical records to be deleted or destroyed prior to the timeframes set out in state legislation and/or our general recommendations.
Aside from the obvious issues relating to continuity of care, you have additional obligations to keep medical records, including Medicare compliance.
Can we delete something that doesn’t belong on the patient’s medical record?
What of the inappropriate and gratuitous commentary noted in the records by Dr Scott’s receptionist?
Most practices have an administrator who can remove or delete entries from a patient’s medical records, but this function is limited for good reason.
On occasion, information that is saved to a medical record doesn’t belong there. In this case, the receptionist has written chapter and verse about how badly Tracey behaved in reception. This resulted in the practice ending care.
The medical record should ultimately benefit the patient and ensure continuity of clinical care. Whilst it might be appropriate to note that care has ended, Dr Scott considered it wasn’t clinically relevant to have included a lengthy and emotive blow-by-blow account.
While removing an entry from a patient’s medical record is not done lightly, it may be reasonable to ‘transfer’ the entry to a more appropriate place. This is often the case in the collection of unsolicited health information. If the information should never have been collected, and does not belong on the medical record, then it can be transferred to a more appropriate location (e.g. the OSH incident reporting file in Tracey’s case) or deleted if it was scanned in by error (e.g. a copy of the practice phone bill).
Take-home message
The OAIC’s Guide to Health Privacy is an excellent resource, but there are some jurisdictional differences – so pay special attention to the examples (in yellow) and helpful hints (in grey). Like unsolicited information, there are a lot of things to think about when considering whether to correct, delete or transfer a medical record, and it is easy to make a bad situation worse – so please contact our Medico-legal Advisory Services team for advice.
Stay updated with the latest medico-legal content |
Subscribe to MDA National’s biannual Member publication, Defence Update, for the latest medico-legal updates, articles and case studies.

Doctors Let's Talk: Get Yourself A Fricking GP
Get yourself a fricking GP stat! is a conversation with Dr Lam, 2019 RACGP National General Practitioner of the Year, rural GP and GP Anesthetics trainee, that explores the importance of finding your own GP as a Junior Doctor.
25 Oct 2022
Systematic efforts to reduce harms due to prescribed opioids – webinar recording
Efforts are underway across the healthcare system to reduce harms caused by pharmaceutical opioids. This 43-min recording of a live webinar, delivered 11 March 2021, is an opportunity for prescribers to check, and potentially improve, their contribution to these endeavours. Hear from an expert panel about recent opioid reforms by the Therapeutic Goods Administration and changes to the Pharmaceutical Benefits Scheme.
14 May 2021
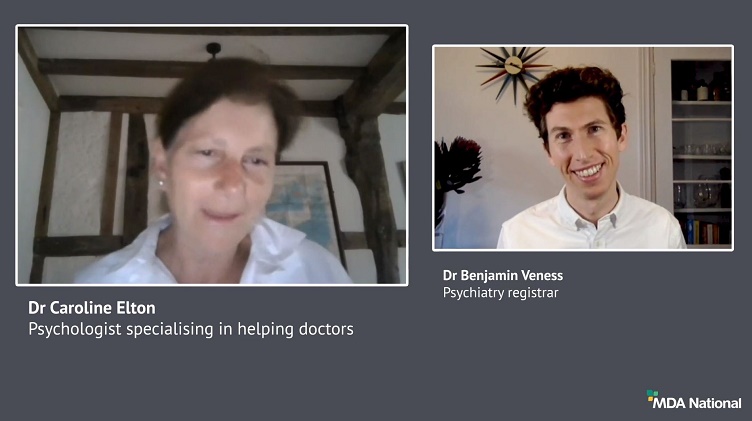
Diplomacy in a hierarchy: tips for approaching a difficult conversation
Have you found yourself wondering how to broach a tough topic of conversation? It can be challenging to effectively navigate a disagreement with a co-worker, especially if they're 'above' you; however, it's vital for positive team dynamics and safe patient care. In this recording of a live webinar you'll have the opportunity to learn from colleagues' experiences around difficult discussions and hear from a diverse panel moderated by Dr Kiely Kim (medico-legal adviser and general practitioner). Recorded live on 2 September 2020.
05 Oct 2020