Using technology for patient care and communication
30 Jan 2023

Can I use SMS to communicate with a patient?
Yes – provided you have the patient’s consent. We recommend you:
- use this type of communication for administrative rather than clinical matters, remembering that an SMS may be seen by someone else
- send the SMS from a practice-dedicated phone or web subscription rather than your personal number
- consider any workplace protocols about the use of SMS and related consent and privacy issues
- save the message to the medical record.
Can I use SMS or apps such as WhatsApp to communicate with colleagues about patients?
Yes, but use with caution. There’s a high risk of a privacy breach because:
- SMS is not encrypted and could be intercepted
- messages on the device may be seen or accessed by someone outside the group
- WhatsApp is encrypted during transmission, but once decrypted on your device the messages may be stored in the cloud on a server overseas
- ex-employees may still have access to group chats.
If your organisation allows it, and you decide the benefits outweigh the risks:
- avoid identifying the patient in the message
- save each message to the patient’s record
- keep your phone secure via settings and strong passwords.
Some healthcare organisations are now using secure clinical communication platforms which allow messaging, group chats and sending images.
Can I use email to communicate with patients?
Yes, if:
- patients consent to it and understand that email isn’t necessarily secure
- there are reasonable IT security measures in place
- you follow workplace protocols
- consent and privacy issues are managed.
Communicating from your personal email address is not recommended.
Emails should be saved in the patient record.
Can I use email to communicate with colleagues about patients?
Yes, if:
- patients consent to it, and understand what information is being sent and that email is not necessarily secure
- you follow workplace protocols
- you manage consent and privacy issues
- there are reasonable IT security measures in place.
Strengthen security by:
- using secure messaging or encrypted email instead of standard unencrypted email
- sending clinical information as a password-protected PDF and sending the password by another means.
Can I use my mobile phone to take clinical photos of patients?
Yes, if the patient consents to it and understands:
- the purpose of taking the photo/s
- who will see the photo/s
- what will be in the photo/s and whether the patient will be identifiable
- how photos will be stored and kept secure, and for how long.
Images where the patient can be identified are subject to the Privacy Act 1988. It’s important to:
- keep your phone as secure as possible via settings and strong passwords
- upload the image to the medical record
- securely delete the image from your phone when it’s no longer needed
- not post images to social media.
Can a consultation be recorded?
Yes, if the patient consents to it and the recording is kept secure. The consent should be written or oral as part of the recording, and the patient should understand:
- what will be recorded and whether they’ll be identifiable
- who will hear the recording
- how it will be stored and for how long
- how they can withdraw their consent.
What do I do if a patient asks to record the consultation?
- Ask the patient why.
- If it’s for a good reason and you’re comfortable with being recorded, you can agree to it.
- If you don’t feel comfortable or don’t think it’s a good idea (e.g. the patient’s condition is sensitive) you can decline. If you decline, you should explain why and offer alternatives such as giving them a written summary or having a family member present during the consultation.
- You may:
- choose to make a recording yourself and keep a copy
- express that you don’t want the recording posted on the internet (including social media) and you could get agreement on this in writing.
- Consider having a practice-wide policy on this issue.
The laws on getting consent for audio and video recordings vary across states and territories. In the Northern Territory, Queensland and Victoria, a patient could legally record and share the recording, including telehealth consultations, without asking you.
Need more specific advice?
- Call 1800 011 255 – available 24 hours a day in an emergency.
- Complete our Contact us form.
- Don’t hesitate to ask us your question, we’re here to support our Members.
References
- Text messaging in general practice – The Royal Australian College of General Practitioners
- General practice ethics: text messages and boundaries in the GP–patient relationship – Australian Family Physician
- The use of communication apps by medical staff in the Australian healthcare system: survey study on prevalence and use – JMIR Med Inform
- Email and texts to patients – MDA National
- Using email in general practice – The Royal Australian College of General Practitioners
- Secure messaging and cyber security for healthcare providers – Australian Digital Health Agency
- Using email in general practice – The Royal Australian College of General Practitioners
- Using personal mobile devices for clinical photos in general practice – The Royal Australian College of General Practitioners
- Taking photos of patients – The Office of the Australian Information Commissioner
- Clinical images and the use of personal mobile devices – Australian Medical Association & Medical Indemnity Industry Association of Australia
- Legal considerations of consent and privacy in the context of clinical photography in Australian medical practice – Med J Aust
- Recording of consults is complex – GPs should proceed with caution – Medical Council of New South Wales
- Making and using visual and audio recordings of patients – General Medical Council (UK)
- Hey doc, I’m recording this consultation – MDA National
Stay updated with the latest medico-legal content |
Subscribe to MDA National’s biannual Member publication, Defence Update, for the latest medico-legal updates, articles and case studies.
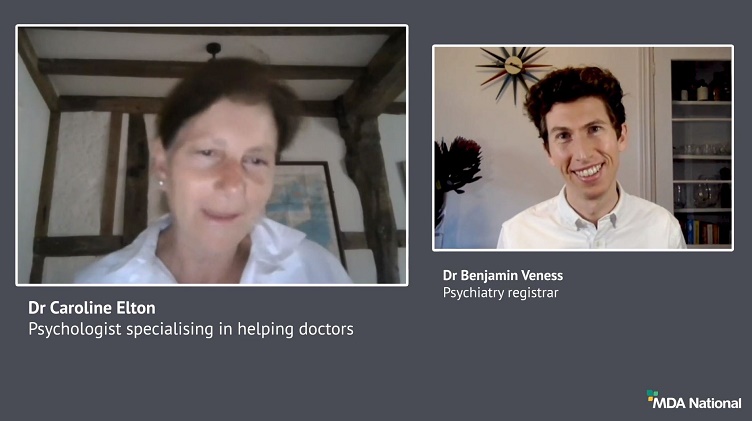
Doctors Let's Talk: Get Yourself A Fricking GP
Get yourself a fricking GP stat! is a conversation with Dr Lam, 2019 RACGP National General Practitioner of the Year, rural GP and GP Anesthetics trainee, that explores the importance of finding your own GP as a Junior Doctor.
25 Oct 2022
Systematic efforts to reduce harms due to prescribed opioids – webinar recording
Efforts are underway across the healthcare system to reduce harms caused by pharmaceutical opioids. This 43-min recording of a live webinar, delivered 11 March 2021, is an opportunity for prescribers to check, and potentially improve, their contribution to these endeavours. Hear from an expert panel about recent opioid reforms by the Therapeutic Goods Administration and changes to the Pharmaceutical Benefits Scheme.
14 May 2021
Diplomacy in a hierarchy: tips for approaching a difficult conversation
Have you found yourself wondering how to broach a tough topic of conversation? It can be challenging to effectively navigate a disagreement with a co-worker, especially if they're 'above' you; however, it's vital for positive team dynamics and safe patient care. In this recording of a live webinar you'll have the opportunity to learn from colleagues' experiences around difficult discussions and hear from a diverse panel moderated by Dr Kiely Kim (medico-legal adviser and general practitioner). Recorded live on 2 September 2020.
05 Oct 2020