The second victim - supporting JMOs through medical errors
08 Dec 2022

The term ‘second victim’, coined by Wu in 2000, encapsulates the impact of medical error on clinicians. Despite public perception, and what hard-line medical culture would have us believe, medical error is inevitable as we are all fallibly human.
We accept the patient as the first victim, and our critical incident review process naturally focuses on their outcomes. But the health professionals who feel responsible can often be neglected.
Although linear root cause analyses attempt to appreciate the multifactorial reasons behind incidents where the individual is only one ‘hole’ in the ‘Swiss Cheese’ model, the emotional impact of errors may be overlooked. Doctors who are second victims may experience psychological distress, burnout, post-traumatic stress, risk-averse practice, and maladaptive behaviours including drug and alcohol abuse, leaving the profession and, in the worst case, suicide.
Junior doctors and trainees (JMOs) are particularly vulnerable to the effects of medical errors. Inexperience, high workload, increased fatigue, burnout, and feelings of inadequate clinical supervision are important contributors. Senior guidance is critical in shifting the perceptive from trauma to growth. Medical errors can be re-envisioned as formative learning experiences – for the second victim, their colleagues and the organisation.
Medical leadership sets the culture for how medical errors are viewed, processed and managed.
The work environment must be a safe place to discuss mistakes. Water-cooler gossip is harmful and should be actively discouraged. JMOs require support when providing open disclosure to the patient, and it helps to understand that admission and apology do not imply legal liability. They should be encouraged to have early discussions with their MDO to address medico-legal consequences.
- Assess any acute needs. Second victims are often distressed immediately after the incident comes to light, needing a safe space for a sounding board and psychological first aid, while steering away from clinical scrutiny. The JMO may need a break or to go home. Disclosing one’s own inevitable experience of medical errors normalises and validates their experience.
- Facilitate reflection to enable clinical growth. Have regular check-ins with the JMO and make sure they know the existing hospital and external support available for further assistance. The DRS4DRS website has many health resources. In times of crisis or distress, this website directs viewers or callers to the state-based doctors' health organisations which provide 24/7 advice lines manned by medical practitioners experienced in doctors' health. These organisations can support doctors acutely, anonymously, and with confidentiality.
Systemic change is needed when approaching medical error. When the second victim is blamed, the healthcare organisation and patients suffer. Consider what simple interventions in everyday practices could prevent future second victims, and integrate early and ongoing support for second victims into the workplace.
Open discussion of medical errors during college education, peer groups and supervision will help dispel the stigma of mistakes. At the end of the day, we are all only human. A human response of empathetic support helps JMOs become better clinicians, moving forward from ‘victim’ to formulating meaning and experience after medical error.
-
References available on request
Stay updated with the latest medico-legal content |
Subscribe to MDA National’s biannual Member publication, Defence Update, for the latest medico-legal updates, articles and case studies.
Doctors Let's Talk: Get Yourself A Fricking GP
Get yourself a fricking GP stat! is a conversation with Dr Lam, 2019 RACGP National General Practitioner of the Year, rural GP and GP Anesthetics trainee, that explores the importance of finding your own GP as a Junior Doctor.
25 Oct 2022
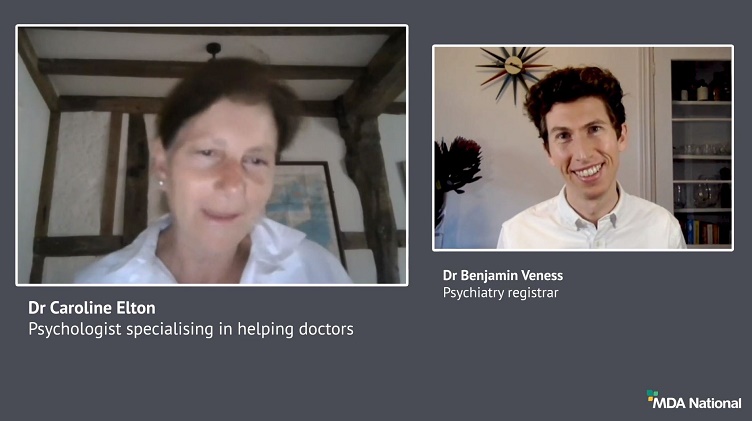
Systematic efforts to reduce harms due to prescribed opioids – webinar recording
Efforts are underway across the healthcare system to reduce harms caused by pharmaceutical opioids. This 43-min recording of a live webinar, delivered 11 March 2021, is an opportunity for prescribers to check, and potentially improve, their contribution to these endeavours. Hear from an expert panel about recent opioid reforms by the Therapeutic Goods Administration and changes to the Pharmaceutical Benefits Scheme.
14 May 2021
Diplomacy in a hierarchy: tips for approaching a difficult conversation
Have you found yourself wondering how to broach a tough topic of conversation? It can be challenging to effectively navigate a disagreement with a co-worker, especially if they're 'above' you; however, it's vital for positive team dynamics and safe patient care. In this recording of a live webinar you'll have the opportunity to learn from colleagues' experiences around difficult discussions and hear from a diverse panel moderated by Dr Kiely Kim (medico-legal adviser and general practitioner). Recorded live on 2 September 2020.
05 Oct 2020